Search
- Page Path
- HOME > Search
- Thyroid
- Active Surveillance for Low-Risk Thyroid Cancers: A Review of Current Practice Guidelines
- Min Joo Kim, Jae Hoon Moon, Eun Kyung Lee, Young Shin Song, Kyong Yeun Jung, Ji Ye Lee, Ji-hoon Kim, Kyungsik Kim, Sue K. Park, Young Joo Park
- Endocrinol Metab. 2024;39(1):47-60. Published online February 15, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1937

- 1,903 View
- 173 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - The indolent nature and favorable outcomes associated with papillary thyroid microcarcinoma have prompted numerous prospective studies on active surveillance (AS) and its adoption as an alternative to immediate surgery in managing low-risk thyroid cancer. This article reviews the current status of AS, as outlined in various international practice guidelines. AS is typically recommended for tumors that measure 1 cm or less in diameter and do not exhibit aggressive subtypes on cytology, extrathyroidal extension, lymph node metastasis, or distant metastasis. To determine the most appropriate candidates for AS, factors such as tumor size, location, multiplicity, and ultrasound findings are considered, along with patient characteristics like medical condition, age, and family history. Moreover, shared decision-making, which includes patient-reported outcomes such as quality of life and cost-effectiveness, is essential. During AS, patients undergo regular ultrasound examinations to monitor for signs of disease progression, including tumor growth, extrathyroidal extension, or lymph node metastasis. In conclusion, while AS is a feasible and reliable approach for managing lowrisk thyroid cancer, it requires careful patient selection, effective communication for shared decision-making, standardized follow-up protocols, and a clear definition of disease progression.

- Diabetes, obesity and metabolism
- Partial Deletion of Perk Improved High-Fat Diet-Induced Glucose Intolerance in Mice
- Jooyeop Lee, Min Joo Kim, Seoil Moon, Ji Yoon Lim, Kyong Soo Park, Hye Seung Jung
- Endocrinol Metab. 2023;38(6):782-787. Published online November 13, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1738
- 722 View
- 45 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
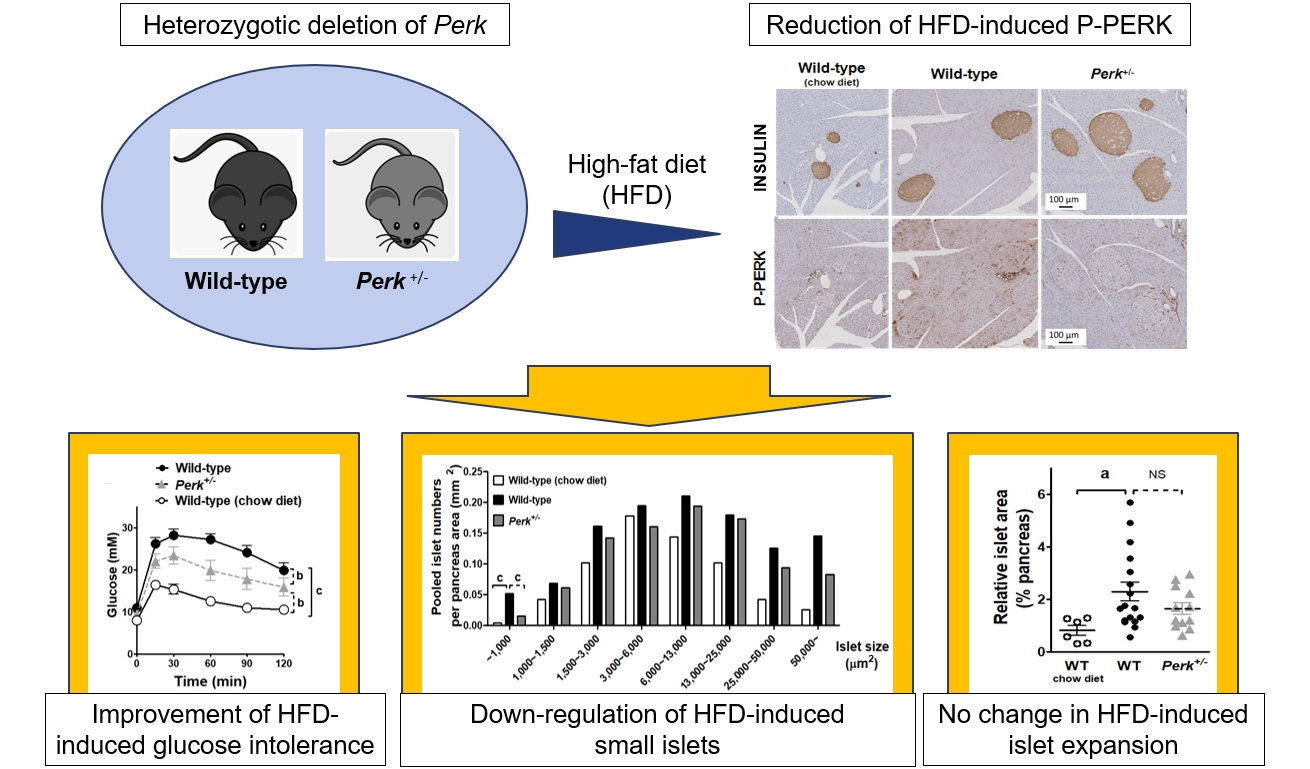
ePub - Although pancreatic endoplasmic reticulum kinase (PERK) is indispensable to beta cells, low-dose PERK inhibitor improved glucose- stimulated insulin secretion (GSIS) and hyperglycemia in diabetic mice. Current study examined if partial deletion of Perk (Perk+/-) recapitulated the effects of PERK inhibitor, on the contrary to the complete deletion. Perk+/- mice and wild-type controls were fed with a high-fat diet (HFD) for 23 weeks. Glucose tolerance was evaluated along with serum insulin levels and islet morphology. Perk+/- mice on normal chow were comparable to wild-type mice in various metabolic features. HFD-induced obesity was not influenced by Perk reduction; however, HFD-induced glucose intolerance was significantly improved since 15-week HFD. HFD-induced compromises in GSIS were relieved by Perk reduction, accompanied by reductions in phosphorylated PERK and activating transcription factor 4 (ATF4) in the islets. Meanwhile, HFD-induced islet expansion was not significantly affected. In summary, partial deletion of Perk improved glucose tolerance and GSIS impaired by diet-induced obesity, without changes in body weights or islet mass.

- Thyroid
- Clinical Outcomes of Repeated Radioactive Iodine Therapy for Graves’ Disease
- Min Joo Kim, Sun Wook Cho, Ye An Kim, Hoon Sung Choi, Young Joo Park, Do Joon Park, Bo Youn Cho
- Endocrinol Metab. 2022;37(3):524-532. Published online June 16, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1418
- 4,843 View
- 230 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
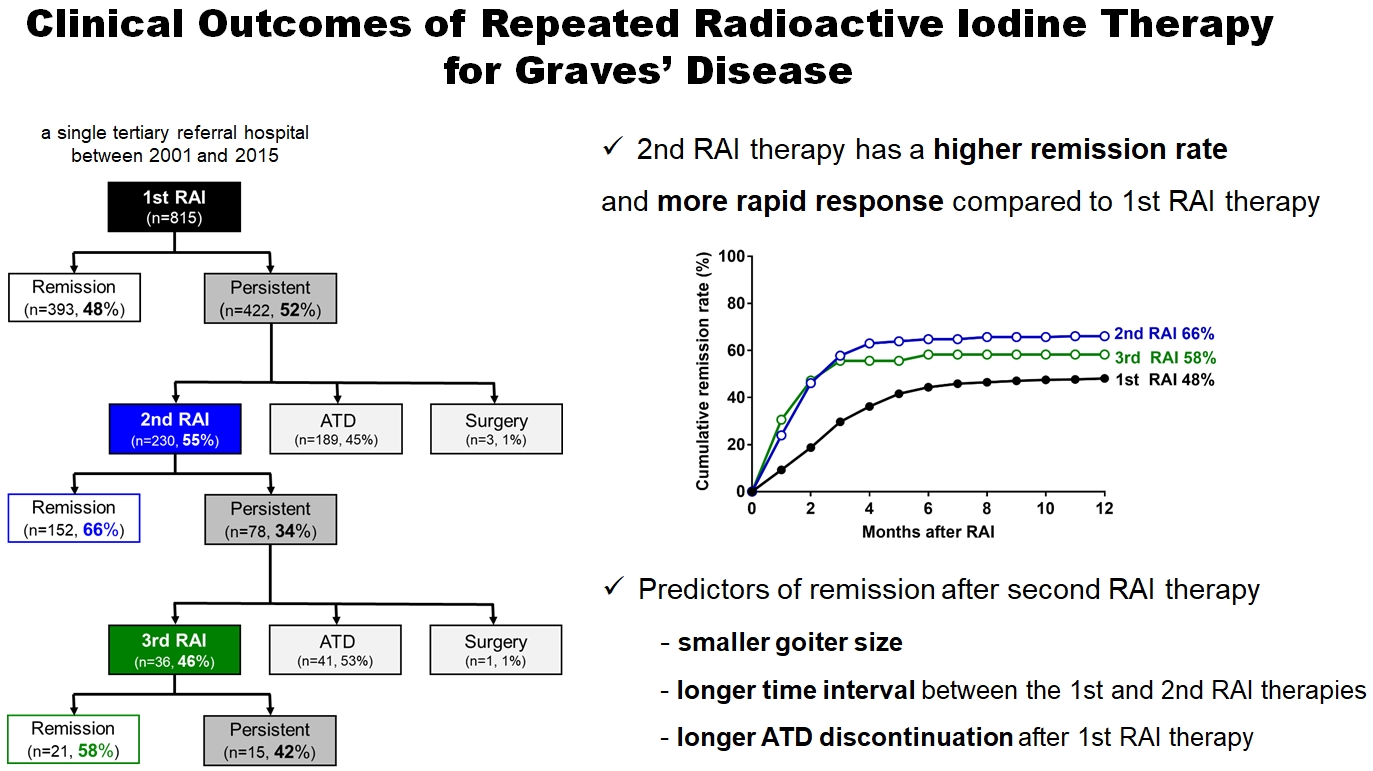
Radioactive iodine (RAI) therapy is a successful therapeutic modality for Graves’ disease. However, RAI therapy can fail, and RAI therapy after antithyroid drugs (ATDs) has a lower remission rate. Therefore, many patients require repeated RAI therapy. This study investigated the clinical outcomes of repeated RAI therapy for Graves’ disease.
Methods
Patients who underwent RAI therapy as second-line therapy after failure of ATD treatment between 2001 and 2015 were reviewed. Remission was defined as hypothyroid or euthyroid status without ATD, and with or without levothyroxine at 12 months after RAI therapy.
Results
The 1-year remission rate after 2nd RAI therapy (66%, 152/230) is significantly higher than that after 1st RAI therapy (48%, 393/815) or long-term ATD treatment after 1st RAI therapy failure (42%). The clinical response to 2nd RAI therapy was more rapid. The median time intervals from the 2nd RAI therapy to ATD discontinuation (1.3 months) and to the start of levothyroxine replacement (2.5 months) were significantly shorter than those for the 1st RAI therapy. A smaller goiter size, a longer time interval between the 1st and 2nd RAI therapies, and a longer ATD discontinuation period predicted remission after the 2nd RAI therapy. Finally, in 78 patients who failed the 2nd RAI therapy, the mean ATD dosage significantly reduced 5.1 mg over 12 months.
Conclusion
Repeated RAI therapy can be a good therapeutic option, especially in patients with smaller goiters and those who are more responsive to the 1st RAI therapy. -
Citations
Citations to this article as recorded by- The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease
Jin Yu, Han-Sang Baek, Chaiho Jeong, Kwanhoon Jo, Jeongmin Lee, Jeonghoon Ha, Min Hee Kim, Jungmin Lee, Dong-Jun Lim
Endocrinology and Metabolism.2023; 38(3): 338. CrossRef - Effect of liver dysfunction on outcome of radioactive iodine therapy for Graves’ disease
Yuyang Ze, Fei Shao, Xuefeng Feng, Shanmei Shen, Yan Bi, Dalong Zhu, Xiaowen Zhang
BMC Endocrine Disorders.2022;[Epub] CrossRef
- The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease

- Thyroid
- Comparison of Korean vs. American Thyroid Imaging Reporting and Data System in Malignancy Risk Assessment of Indeterminate Thyroid Nodules
- Sunyoung Kang, Seul Ki Kwon, Hoon Sung Choi, Min Joo Kim, Young Joo Park, Do Joon Park, Sun Wook Cho
- Endocrinol Metab. 2021;36(5):1111-1120. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1208
- 4,001 View
- 127 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
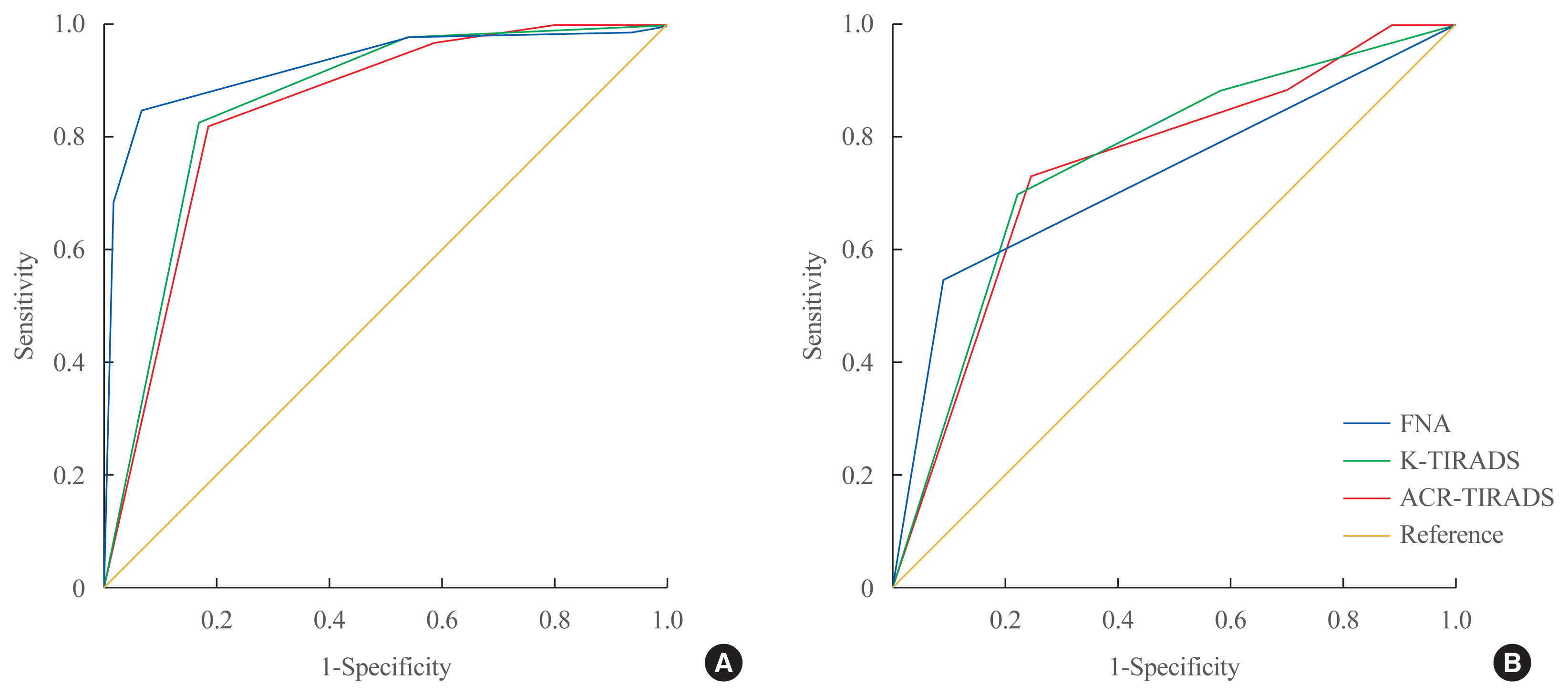
The management of cytologically indeterminate thyroid nodules is challenging for clinicians. This study aimed to compare the diagnostic performance of the Korean Thyroid Imaging Reporting and Data Systems (K-TIRADS) with that of the American College of Radiology (ACR)-TIRADS for predicting the malignancy risk of indeterminate thyroid nodules.
Methods
Thyroid nodules diagnosed by fine-needle aspiration (FNA) followed by surgery or core needle biopsy at a single referral hospital were enrolled.
Results
Among 200 thyroid nodules, 78 (39.0%) nodules were classified as indeterminate by FNA (Bethesda category III, IV, and V), and 114 (57.0%) nodules were finally diagnosed as malignancy by surgery or core needle biopsy. The area under the curve (AUC) was higher for FNA than for either TIRADS system in all nodules, while all three methods showed similar AUCs for indeterminate nodules. However, for Bethesda category III nodules, applying K-TIRADS 5 significantly increased the risk of malignancy compared to a cytological examination alone (50.0% vs. 26.5%, P=0.028), whereas applying ACR-TIRADS did not lead to a change.
Conclusion
K-TIRADS and ACR-TIRADS showed similar diagnostic performance in assessing indeterminate thyroid nodules, and K-TIRADS had beneficial effects for malignancy prediction in Bethesda category III nodules. -
Citations
Citations to this article as recorded by- Is the nodule location a predictive risk factor for cancer in AUS/FLUS thyroid nodules? A retrospective cohort study
Saad M. Alqahtani, Bassam A. Altalhi, Yousef S. Alalawi, Saif S. Al-Sobhi
Asian Journal of Surgery.2024;[Epub] CrossRef - Diagnostic Performance of Various Ultrasound Risk Stratification Systems for Benign and Malignant Thyroid Nodules: A Meta-Analysis
Ji-Sun Kim, Byung Guk Kim, Gulnaz Stybayeva, Se Hwan Hwang
Cancers.2023; 15(2): 424. CrossRef - The impact of thyroid imaging reporting and data system on the management of Bethesda III thyroid nodules
Saad M. Alqahtani, Saif S. Al-Sobhi, Mohammed A. Alturiqy, Riyadh I. Alsalloum, Hindi N. Al-Hindi
Journal of Taibah University Medical Sciences.2023; 18(3): 506. CrossRef - Diagnostic Performance of Six Ultrasound Risk Stratification Systems for Thyroid Nodules: A Systematic Review and Network Meta-Analysis
Do Hyun Kim, Sung Won Kim, Mohammed Abdullah Basurrah, Jueun Lee, Se Hwan Hwang
American Journal of Roentgenology.2023; 220(6): 791. CrossRef - Diagnostic efficiency among Eu-/C-/ACR-TIRADS and S-Detect for thyroid nodules: a systematic review and network meta-analysis
Longtao Yang, Cong Li, Zhe Chen, Shaqi He, Zhiyuan Wang, Jun Liu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Comparison of diagnostic performance of two ultrasound risk stratification systems for thyroid nodules: a systematic review and meta-analysis
Yun Jin Kang, Hee Sun Ahn, Gulnaz Stybayeva, Ju Eun Lee, Se Hwan Hwang
La radiologia medica.2023; 128(11): 1407. CrossRef - Diagnostic Performance of ACR and Kwak TI-RADS for Benign and Malignant Thyroid Nodules: An Update Systematic Review and Meta-Analysis
Yun Jin Kang, Gulnaz Stybayeya, Ju Eun Lee, Se Hwan Hwang
Cancers.2022; 14(23): 5961. CrossRef - Comparison of Thyroid Imaging Reporting and Data Systems in Malignancy Risk Stratification of Indeterminate Thyroid Nodules
Bo Hyun Kim
Endocrinology and Metabolism.2021; 36(5): 974. CrossRef
- Is the nodule location a predictive risk factor for cancer in AUS/FLUS thyroid nodules? A retrospective cohort study

- Endocrine Research
- DEHP Down-Regulates Tshr Gene Expression in Rat Thyroid Tissues and FRTL-5 Rat Thyrocytes: A Potential Mechanism of Thyroid Disruption
- Min Joo Kim, Hwan Hee Kim, Young Shin Song, Ok-Hee Kim, Kyungho Choi, Sujin Kim, Byung-Chul Oh, Young Joo Park
- Endocrinol Metab. 2021;36(2):447-454. Published online March 31, 2021
- DOI: https://doi.org/10.3803/EnM.2020.920
- 5,054 View
- 145 Download
- 12 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
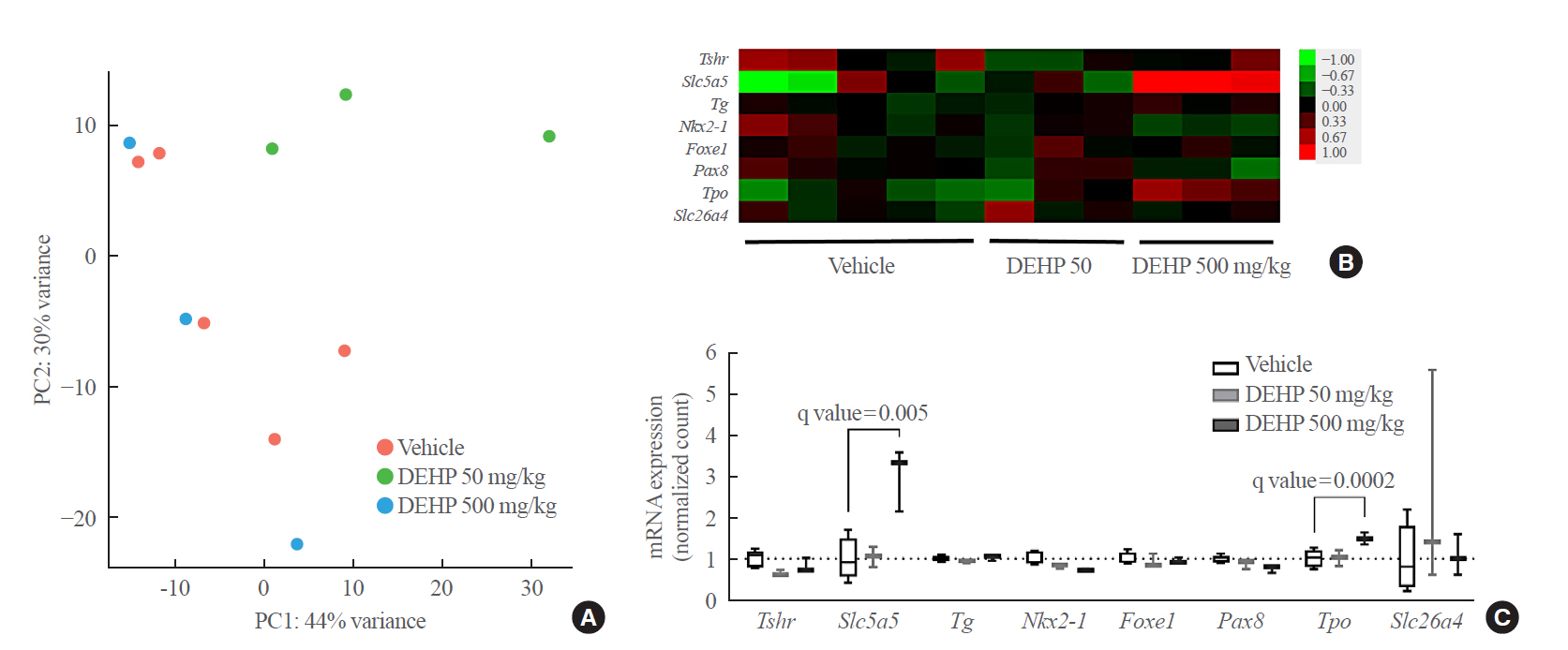
Di-2-ethylhexyl phthalate (DEHP) is known to disrupt thyroid hormonal status. However, the underlying molecular mechanism of this disruption is unclear. Therefore, we investigated the direct effects of DEHP on the thyroid gland.
Methods
DEHP (vehicle, 50 mg/kg, and 500 mg/kg) was administered to Sprague-Dawley rats for 2 weeks. The expression of the thyroid hormone synthesis pathway in rat thyroid tissues was analyzed through RNA sequencing analysis, quantitative reverse transcription-polymerase chain reaction (RT-PCR), and immunohistochemical (IHC) staining. DEHP was treated to FRTL-5 rat thyroid cells, and an RT-PCR analysis was performed. A reporter gene assay containing the promoter of thyroid stimulating hormone receptor (TSHR) in Nthy-ori 3-1 human thyroid cells was constructed, and luciferase activity was determined.
Results
After DEHP treatment, the free thyroxine (T4) and total T4 levels in rats significantly decreased. RNA sequencing analysis of rat thyroid tissues showed little difference between vehicle and DEHP groups. In the RT-PCR analysis, Tshr expression was significantly lower in both DEHP groups (50 and 500 mg/kg) compared to that in the vehicle group, and IHC staining showed that TSHR expression in the 50 mg/kg DEHP group significantly decreased. DEHP treatment to FRTL-5 cells significantly down-regulated Tshr expression. DEHP treatment also reduced luciferase activity in a reporter gene assay for TSHR.
Conclusion
Although overall genetic changes in the thyroid hormone synthesis pathway are not clear, DEHP exposure could significantly down-regulate Tshr expression in thyroid glands. Down-regulation of Tshr gene appears to be one of potential mechanisms of thyroid disruption by DEHP exposure. -
Citations
Citations to this article as recorded by- ARTS is essential for di-2-ethylhexyl phthalate (DEHP)-induced apoptosis of mouse Leydig cells
Yue Li, Linlin Xu, Chaoju Hao, Si Yang, Jinglei Wang, Jiaxiang Chen
Ecotoxicology and Environmental Safety.2024; 270: 115882. CrossRef - Thyroid dysfunction caused by exposure to environmental endocrine disruptors and the underlying mechanism: A review
Jie He, Jie Xu, Mucong Zheng, Kai Pan, Lilin Yang, Lina Ma, Chuyang Wang, Jie Yu
Chemico-Biological Interactions.2024; 391: 110909. CrossRef - Intrauterine exposure to di(2-ethylhexyl) phthalate (DEHP) disrupts the function of the hypothalamus-pituitary-thyroid axis of the F1 rats during adult life
Érica Kássia Sousa-Vidal, Guilherme Henrique, Renata Elen Costa da Silva, Caroline Serrano-Nascimento
Frontiers in Endocrinology.2023;[Epub] CrossRef - Drinking water disinfection byproduct iodoacetic acid affects thyroid hormone synthesis in Nthy-ori 3–1 cells
Jingyi Xiao, Yujie Sha, Yuwen Huang, Kunling Long, Huan Wu, Yan Mo, Qiyuan Yang, Shengkun Dong, Qiang Zeng, Xiao Wei
Ecotoxicology and Environmental Safety.2023; 257: 114926. CrossRef - Assessment of five typical environmental endocrine disruptors and thyroid cancer risk: a meta-analysis
Yuyao Yang, Xiaoyue Bai, Juan Lu, Ronghao Zou, Rui Ding, Xiaohui Hua
Frontiers in Endocrinology.2023;[Epub] CrossRef - Investigation of the effects of phthalates on in vitro thyroid models with RNA-Seq and ATAC-Seq
Marta Nazzari, Mírian Romitti, Duncan Hauser, Daniel J. Carvalho, Stefan Giselbrecht, Lorenzo Moroni, Sabine Costagliola, Florian Caiment
Frontiers in Endocrinology.2023;[Epub] CrossRef - Di(2-ethylhexyl) phthalate (DEHP) and thyroid: biological mechanisms of interference and possible clinical implications
Xueting Zhang, Wen Qi, Qi Xu, Xu Li, Liting Zhou, Lin Ye
Environmental Science and Pollution Research.2022; 29(2): 1634. CrossRef - The possible thyroid disruptive effect of di-(2-ethyl hexyl) phthalate and the potential protective role of selenium and curcumin nanoparticles: a toxicological and histological study
Naima Abd El-Halim Sherif, Asmaa El-Banna, Rehab Ahmed Abdel-Moneim, Zahraa Khalifa Sobh, Manal Ibrahim Fathy Balah
Toxicology Research.2022; 11(1): 108. CrossRef - Environmental disruption of reproductive rhythms
Marie-Azélie Moralia, Clarisse Quignon, Marine Simonneaux, Valérie Simonneaux
Frontiers in Neuroendocrinology.2022; 66: 100990. CrossRef - Endocrine-disruptor endpoints in the ovary and thyroid of adult female rats exposed to realistic doses of di-(2-ethylhexyl) phthalate
Amel Jebara, Asma Beltifa, Guissepa Di Bella, Lotfi Mabrouk, Hedi Ben Mansour
Journal of Water and Health.2022; 20(8): 1256. CrossRef - The influence of sunitinib and sorafenib, two tyrosine kinase inhibitors, on development and thyroid system in zebrafish larvae
Gang Wei, Cao-xu Zhang, Yu Jing, Xia Chen, Huai-dong Song, Liu Yang
Chemosphere.2022; 308: 136354. CrossRef - Role of estrogen receptors in thyroid toxicity induced by mono (2-ethylhexyl) phthalate via endoplasmic reticulum stress: An in vitro mechanistic investigation
Qi Xu, Liting Zhou, Hyonju Ri, Xu Li, Xueting Zhang, Wen Qi, Lin Ye
Environmental Toxicology and Pharmacology.2022; 96: 104007. CrossRef
- ARTS is essential for di-2-ethylhexyl phthalate (DEHP)-induced apoptosis of mouse Leydig cells

- Clinical Study
- Low Predictive Value of FRAX Adjusted by Trabecular Bone Score for Osteoporotic Fractures in Korean Women: A Community-Based Cohort Study
- Hana Kim, Jung Hee Kim, Min Joo Kim, A Ram Hong, HyungJin Choi, EuJeong Ku, Ji Hyun Lee, Chan Soo Shin, Nam H. Cho
- Endocrinol Metab. 2020;35(2):359-366. Published online June 24, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.2.359
- 5,938 View
- 132 Download
- 9 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
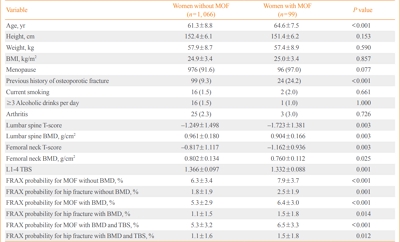
ePub - Background
The value of the Fracture Risk Assessment Tool (FRAX) and the trabecular bone score (TBS) for assessing osteoporotic fracture risk has not been fully elucidated in Koreans. We conducted this study to clarify the predictive value of FRAX adjusted by TBS for osteoporotic fractures in Korean women.
Methods
After screening 7,192 eligible subjects from the Ansung cohort, 1,165 women aged 45 to 76 years with available bone mineral density (BMD) and TBS data were enrolled in this study. We assessed their clinical risk factors for osteoporotic fractures and evaluated the predictive value of FRAX with or without BMD and TBS.
Results
During the mean follow-up period of 7.5 years, 99 (8.5%) women suffered major osteoporotic fractures (MOFs) and 28 (2.4%) experienced hip fractures. FRAX without BMD, BMD-adjusted FRAX, and TBS-adjusted FRAX were significantly associated with the risk of MOFs (hazard ratio [HR] per percent increase, 1.08; 95% confidence interval [CI], 1.03 to 1.14; HR, 1.09; 95% CI, 1.03 to 1.15; and HR, 1.07; 95% CI, 1.02 to 1.13, respectively). However, BMD-adjusted FRAX and TBS-adjusted FRAX did not predict MOFs better than FRAX without BMD based on the Harrell’s C statistic. FRAX probabilities showed limited value for predicting hip fractures. The cut-off values of FRAX without BMD, FRAX with BMD, and FRAX with BMD adjusted by TBS for predicting MOFs were 7.2%, 5.0%, and 6.7%, respectively.
Conclusion
FRAX with BMD and TBS adjustment did not show better predictive value for osteoporotic fractures in this study than FRAX without adjustment. Moreover, the cut-off values of FRAX probabilities for treatment might be lower in Korean women than in other countries. -
Citations
Citations to this article as recorded by- Update on the utility of trabecular bone score (TBS) in clinical practice for the management of osteoporosis: a systematic review by the Egyptian Academy of Bone and Muscle Health
Yasser El Miedany, Walaa Elwakil, Mohammed Hassan Abu-Zaid, Safaa Mahran
Egyptian Rheumatology and Rehabilitation.2024;[Epub] CrossRef - Comparison of predictive value of FRAX, trabecular bone score, and bone mineral density for vertebral fractures in systemic sclerosis: A cross-sectional study
Kyung-Ann Lee, Hyun-Joo Kim, Hyun-Sook Kim
Medicine.2023; 102(2): e32580. CrossRef - Screening for the primary prevention of fragility fractures among adults aged 40 years and older in primary care: systematic reviews of the effects and acceptability of screening and treatment, and the accuracy of risk prediction tools
Michelle Gates, Jennifer Pillay, Megan Nuspl, Aireen Wingert, Ben Vandermeer, Lisa Hartling
Systematic Reviews.2023;[Epub] CrossRef - Chronic airway disease as a major risk factor for fractures in osteopenic women: Nationwide cohort study
Sung Hye Kong, Ae Jeong Jo, Chan Mi Park, Kyun Ik Park, Ji Eun Yun, Jung Hee Kim
Frontiers in Endocrinology.2023;[Epub] CrossRef - Update on the clinical use of trabecular bone score (TBS) in the management of osteoporosis: results of an expert group meeting organized by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Disease
Enisa Shevroja, Jean-Yves Reginster, Olivier Lamy, Nasser Al-Daghri, Manju Chandran, Anne-Laurence Demoux-Baiada, Lynn Kohlmeier, Marie-Paule Lecart, Daniel Messina, Bruno Muzzi Camargos, Juraj Payer, Sansin Tuzun, Nicola Veronese, Cyrus Cooper, Eugene V.
Osteoporosis International.2023; 34(9): 1501. CrossRef - Comparison of HU histogram analysis and BMD for proximal femoral fragility fracture assessment: a retrospective single-center case–control study
Sun-Young Park, Hong Il Ha, Injae Lee, Hyun Kyung Lim
European Radiology.2022; 32(3): 1448. CrossRef - Association of Trabecular Bone Score-Adjusted Fracture Risk Assessment Tool with Coronary Artery Calcification in Women
Tzyy-Ling Chuang, Yuh-Feng Wang, Malcolm Koo, Mei-Hua Chuang
Diagnostics.2022; 12(1): 178. CrossRef - Risk of osteoporotic fracture in women using the FRAX tool with and without bone mineral density score in patients followed at a tertiary outpatient clinic ‒ An observational study
Maria Helena Sampaio Favarato, Maria Flora de Almeida, Arnaldo Lichtenstein, Milton de Arruda Martins, Mario Ferreira Junior
Clinics.2022; 77: 100015. CrossRef - Comparison of Trabecular Bone Score–Adjusted Fracture Risk Assessment (TBS-FRAX) and FRAX Tools for Identification of High Fracture Risk among Taiwanese Adults Aged 50 to 90 Years with or without Prediabetes and Diabetes
Tzyy-Ling Chuang, Mei-Hua Chuang, Yuh-Feng Wang, Malcolm Koo
Medicina.2022; 58(12): 1766. CrossRef - Application of the Trabecular Bone Score in Clinical Practice
Sung Hye Kong, Namki Hong, Jin-Woo Kim, Deog Yoon Kim, Jung Hee Kim
Journal of Bone Metabolism.2021; 28(2): 101. CrossRef
- Update on the utility of trabecular bone score (TBS) in clinical practice for the management of osteoporosis: a systematic review by the Egyptian Academy of Bone and Muscle Health

- Thyroid
- Bisphenols and Thyroid Hormone
- Min Joo Kim, Young Joo Park
- Endocrinol Metab. 2019;34(4):340-348. Published online December 23, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.4.340
- 9,099 View
- 235 Download
- 60 Web of Science
- 64 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub In recent decades, attention has been directed toward the effects of bisphenol A (BPA) on human health. BPA has estrogenic activity and is regarded as a representative endocrine disruptor. In addition, mounting evidence indicates that BPA can disrupt thyroid hormone and its action. This review examined human epidemiological studies to investigate the association between BPA exposure and thyroid hormone levels, and analyzed
in vivo andin vitro experiments to identify the causal relationship and its mechanism of action. BPA is involved in thyroid hormone action not only as a thyroid hormone receptor antagonist, but also through several other mechanisms. Since the use of bisphenols other than BPA has recently increased, we also reviewed the effects of other bisphenols on thyroid hormone action.-
Citations
Citations to this article as recorded by- The Role of Endocrine Disruptors Bisphenols and Phthalates in Obesity: Current Evidence, Perspectives and Controversies
Maria Dalamaga, Dimitrios Kounatidis, Dimitrios Tsilingiris, Natalia G. Vallianou, Irene Karampela, Sotiria Psallida, Athanasios G. Papavassiliou
International Journal of Molecular Sciences.2024; 25(1): 675. CrossRef - Environmental toxicology of bisphenol A: Mechanistic insights and clinical implications on the neuroendocrine system
Tongbing Qi, Dongqing Jing, Kexin Zhang, Junfeng Shi, Hongyan Qiu, Chengxia Kan, Fang Han, Chunyan Wu, Xiaodong Sun
Behavioural Brain Research.2024; 460: 114840. CrossRef - Antioxidant compounds from the Arthrospira platensis protect against Bisphenol A-induced nephrotoxicity in rats
Khadidja Chouala, Kahina Boudjema, Yahia Khelef, Sadok Nani, Kheireddine Ouali, Mahieddine Boumendjel, Amel Boumendjel, Mahfoud Messarah
Toxicology and Environmental Health Sciences.2024; 16(1): 75. CrossRef - Associations of urinary non-persistent endocrine disrupting chemical biomarkers with early-to-mid pregnancy plasma sex-steroid and thyroid hormones
Brad A. Ryva, Diana C. Pacyga, Kaitlyn Y. Anderson, Antonia M. Calafat, Jason Whalen, Max T. Aung, Joseph C. Gardiner, Joseph M. Braun, Susan L. Schantz, Rita S. Strakovsky
Environment International.2024; 183: 108433. CrossRef - Prospective role of lusianthridin in attenuating cadmium-induced functional and cellular damage in rat thyroid
Teng Gao, Sijia Luo, Hongguang Li, Zijie Su, Qinghui Wen
Heliyon.2024; 10(5): e27080. CrossRef - Exposure to Bisphenol A, S, and F and its Association with Obesity and Diabetes Mellitus in General Adults of Korea: Korean National Environmental Health Survey (KoNEHS) 2015–2017
Min Kyong Moon, Min Joo Kim, Inae Lee, Sunmi Kim, Sohyeon Choi, Jeongim Park, Yoon Hee Cho, Sooyeon Hong, Jiyoung Yoo, Hyunwoong Park, Gi Jeong Cheon, Young Joo Park, Kyungho Choi
Exposure and Health.2023; 15(1): 53. CrossRef - Exposure to Bisphenol A increases malignancy risk of thyroid nodules in overweight/obese patients
Vincenzo Marotta, Lucia Grumetto, Ilaria Neri, Giacomo Russo, Anna Tortora, Giulia Izzo, Ilaria Panariello, Domenico Rocco, Luciano Pezzullo, Mario Vitale
Environmental Pollution.2023; 316: 120478. CrossRef - A case-control study of urinary concentrations of bisphenol A, bisphenol F, and bisphenol S and the risk of papillary thyroid cancer
Lei Zhang, Jiahuai Zhang, Sai Fan, Yuxin Zhong, Jingguang Li, Yunfeng Zhao, Song Ni, Jiaying Liu, Yongning Wu
Chemosphere.2023; 312: 137162. CrossRef - Endocrine disruptors and endometriosis
Sudipta Dutta, Sakhila K. Banu, Joe A. Arosh
Reproductive Toxicology.2023; 115: 56. CrossRef - Bisphenol A alternatives continuously contribute to the endocrine disruption in cetaceans
Yongwei Guo, Wei Shi, Zhiwei Liu, Xian Sun, Jiaxue Wu, Yuping Wu
Environment International.2023; 171: 107679. CrossRef - Environmental endocrine disruptors and amphibian immunity: A bridge between the thyroid hormone axis and T cell development
Connor C. McGuire, Jacques R. Robert
Developmental & Comparative Immunology.2023; 140: 104617. CrossRef - Transient developmental exposure to low doses of bisphenol F negatively affects neurogliogenesis and olfactory behaviour in adult mice
Pieter Vancamp, Lucile Butruille, Anni Herranen, Anita Boelen, Jean-Baptiste Fini, Barbara A. Demeneix, Sylvie Remaud
Environment International.2023; 172: 107770. CrossRef - A Fast Method for Determination of Seven Bisphenols in Human Breast Milk Samples with the Use of HPLC-FLD
Szymon Szubartowski, Tomasz Tuzimski
Molecules.2023; 28(3): 1432. CrossRef - Risk Assessment of Bisphenol A in the Korean General Population
Myungsil Hwang, Seon-Joo Park, Hae-Jeung Lee
Applied Sciences.2023; 13(6): 3587. CrossRef - Current Evidence on Bisphenol A Exposure and the Molecular Mechanism Involved in Related Pathological Conditions
Ylenia Della Rocca, Enrico Matteo Traini, Francesca Diomede, Luigia Fonticoli, Oriana Trubiani, Alessia Paganelli, Jacopo Pizzicannella, Guya Diletta Marconi
Pharmaceutics.2023; 15(3): 908. CrossRef - The associations between concentrations of gestational bisphenol analogues and thyroid related hormones in cord blood: A prospective cohort study
Jianya Xi, Xiujuan Su, Ziliang Wang, Honglei Ji, Yao Chen, Xiaofang Liu, Maohua Miao, Hong Liang, Wei Yuan
Ecotoxicology and Environmental Safety.2023; 256: 114838. CrossRef - Zebrafish (Danio rerio) TRβ- and TTR-based electrochemical biosensors: Construction and application for the evaluation of thyroid-disrupting activity of bisphenols
Yuejiao Li, Zhenzhong Zhang, Jun Wang, Yeqi Shan, Hua Tian, Pengfei Cui, Shaoguo Ru
Environmental Pollution.2023; 330: 121745. CrossRef - Iodine Deficiency, Maternal Hypothyroxinemia and Endocrine Disrupters Affecting Fetal Brain Development: A Scoping Review
Rolf Grossklaus, Klaus-Peter Liesenkötter, Klaus Doubek, Henry Völzke, Roland Gaertner
Nutrients.2023; 15(10): 2249. CrossRef - Bisphenol A Analogues Inhibit Human and Rat 11β-Hydroxysteroid Dehydrogenase 1 Depending on Its Lipophilicity
Hong Wang, Jianmin Sang, Zhongyao Ji, Yang Yu, Shaowei Wang, Yang Zhu, Huitao Li, Yiyan Wang, Qiqi Zhu, Renshan Ge
Molecules.2023; 28(13): 4894. CrossRef - Bisphenol A-Induced Endocrine Dysfunction and its Associated Metabolic Disorders
Meenu Maniradhan, Latchoumycandane Calivarathan
Endocrine, Metabolic & Immune Disorders - Drug Targets.2023; 23(4): 515. CrossRef - Origin, dietary exposure, and toxicity of endocrine-disrupting food chemical contaminants: A comprehensive review
Leila Peivasteh-roudsari, Raziyeh Barzegar-bafrouei, Kurush Aghbolagh Sharifi, Shamimeh Azimisalim, Marziyeh Karami, Solmaz Abedinzadeh, Shabnam Asadinezhad, Behrouz Tajdar-oranj, Vahideh Mahdavi, Adel Mirza Alizadeh, Parisa Sadighara, Margherita Ferrante
Heliyon.2023; 9(7): e18140. CrossRef - Bisphenol analogues induce thyroid dysfunction via the disruption of the thyroid hormone synthesis pathway
Chao Hu, Yeqing Xu, Mingmin Wang, Shixuan Cui, Hangjun Zhang, Liping Lu
Science of The Total Environment.2023; 900: 165711. CrossRef - Distinct inhibitory strength of bisphenol A analogues on human and rat 11β-hydroxysteroid dehydrogenase 1: 3D quantitative structure-activity relationship and in silico molecular docking analysis
Han Lu, Shaowei Wang, Jingyi Zheng, Yang Zhu, Yiyan Wang, Huitao Li, Ren-shan Ge
Ecotoxicology and Environmental Safety.2023; 267: 115638. CrossRef - Systematic Review on Safety of Bisphenol A: from Invention to the Present
Hananeh KORDBACHEH, Bensu KARAHALİL
Eurasian Journal of Toxicology.2023; 5(2): 37. CrossRef - Bisphenol S dysregulates thyroid hormone homeostasis; Testicular survival, redox and metabolic status: Ameliorative actions of melatonin
Aishwarya Sahu, Rakesh Verma
Environmental Toxicology and Pharmacology.2023; 104: 104300. CrossRef - Structural binding perspectives of common plasticizers and a flame retardant, BDE‐153, against thyroxine‐binding globulin: potential for endocrine disruption
Ishfaq Ahmad Sheikh, Mohd Amin Beg
Journal of Applied Toxicology.2022; 42(5): 841. CrossRef - New insights on the effects of endocrine-disrupting chemicals on children
Barbara Predieri, Crésio A.D. Alves, Lorenzo Iughetti
Jornal de Pediatria.2022; 98: S73. CrossRef - Toxic Metal Concentrations in Drinking Water and Possible Effect on Sex Hormones among Men in Sabongida-Ora, Edo State, Nigeria
Osaro Ogie Enehizena, Mathias A. Emokpae
Medicines.2022; 9(1): 4. CrossRef - Bisphenols impact hormone levels in animals: A meta-analysis
Alexander M. Rubin, Frank Seebacher
Science of The Total Environment.2022; 828: 154533. CrossRef - The effects of prenatal and lactational bisphenol A and/or di(2-ethylhexyl) phthalate exposure on female reproductive system
Gizem Ozkemahli, Aylin Balci Ozyurt, Pinar Erkekoglu, Naciye Dilara Zeybek, Nilgun Yersal, Belma Kocer-Gumusel
Toxicology Mechanisms and Methods.2022; 32(8): 597. CrossRef - Associations of Phthalate Metabolites and Bisphenol A Levels with Obesity in Children: The Korean National Environmental Health Survey (KoNEHS) 2015 to 2017
Moon Young Seo, Shinje Moon, Shin-Hye Kim, Mi Jung Park
Endocrinology and Metabolism.2022; 37(2): 249. CrossRef - Associations of bisphenol exposure with thyroid hormones in pregnant women: a prospective birth cohort study in China
Huishen Huang, Jun Liang, Peng Tang, Chuanxiang Yu, Haoran Fan, Qian Liao, Jinghua Long, Dongxiang Pan, Xiaoyun Zeng, Shun Liu, Dongping Huang, Xiaoqiang Qiu
Environmental Science and Pollution Research.2022; 29(58): 87170. CrossRef - Bisphenols A, F, S and AF trigger apoptosis and/or endoplasmic reticulum stress in human endometrial stromal cells
Ricardo Ferreira, Cristina Amaral, Georgina Correia-da-Silva, Marta Almada, Margarida Borges, Sara Cristina Cunha, José Oliveira Fernandes, Natércia Teixeira
Toxicology.2022; 478: 153282. CrossRef - Association between phenols and thyroid hormones: The role of iodothyronine deiodinase genes
Blanca Sarzo, Reem Abumallouh, Natalia Marín, Sabrina Llop, Andrea Beneito, Inmaculada Lopez-Flores, Nerea Ferrero, Amrit Kaur Sakhi, Ferran Ballester, Maria-Jose Lopez-Espinosa
Environmental Pollution.2022; 311: 119926. CrossRef - Bisphenol A as a Factor in the Mosaic of Autoimmunity
Zora Lazurova, Ivica Lazurova, Yehuda Shoenfeld
Endocrine, Metabolic & Immune Disorders - Drug Targets.2022; 22(7): 728. CrossRef - Zebrafish as an emerging tool for drug discovery and development for thyroid diseases
Poonam Yadav, Lopmudra P. Sarode, Ravinder Reddy Gaddam, Puneet Kumar, Jasvinder Singh Bhatti, Amit Khurana, Umashanker Navik
Fish & Shellfish Immunology.2022; 130: 53. CrossRef - Review of in silico studies dedicated to the nuclear receptor family: Therapeutic prospects and toxicological concerns
Asma Sellami, Manon Réau, Matthieu Montes, Nathalie Lagarde
Frontiers in Endocrinology.2022;[Epub] CrossRef - Use of high-resolution metabolomics to assess the biological perturbations associated with maternal exposure to Bisphenol A and Bisphenol F among pregnant African American women
Rachel Tchen, Youran Tan, Dana Boyd Barr, P. Barry Ryan, ViLinh Tran, Zhenjiang Li, Yi-Juan Hu, Alicia K. Smith, Dean P. Jones, Anne L. Dunlop, Donghai Liang
Environment International.2022; 169: 107530. CrossRef - Effects of bisphenol A on pancreas and thyroid gland of young and adult female Sprague Dawlеy rats
D. Yahia, H. Hamdy, D. A. Salem, S. Afifi
BULGARIAN JOURNAL OF VETERINARY MEDICINE.2022; 25(3): 426. CrossRef - Bisphenol A analogues induce a feed-forward estrogenic response in zebrafish
Silvia Karim, Ruixin Hao, Caroline Pinto, Jan-Åke Gustafsson, Marina Grimaldi, Patrick Balaguer, Maria Bondesson
Toxicology and Applied Pharmacology.2022; 455: 116263. CrossRef - Mediterranean Diet and Thyroid: An Interesting Alliance
Giuseppe Bellastella, Lorenzo Scappaticcio, Francesco Caiazzo, Maria Tomasuolo, Raffaela Carotenuto, Mariangela Caputo, Stefania Arena, Paola Caruso, Maria Ida Maiorino, Katherine Esposito
Nutrients.2022; 14(19): 4130. CrossRef - Endocrine Disrupting Chemicals’ Effects in Children: What We Know and What We Need to Learn?
Barbara Predieri, Lorenzo Iughetti, Sergio Bernasconi, Maria Elisabeth Street
International Journal of Molecular Sciences.2022; 23(19): 11899. CrossRef - Single and repeated bisphenol A treatment induces ROS, Aβ and hyperphosphorylated-tau accumulation, and insulin pathways disruption, through HDAC2 and PTP1B overexpression, leading to SN56 cholinergic apoptotic cell death
Andrea Flores, Paula Moyano, Emma Sola, José Manuel García, Jimena García, María José Anadon, María Teresa Frejo, Maria Victoria Naval, Maria de la Cabeza Fernadez, Javier del Pino
Food and Chemical Toxicology.2022; 170: 113500. CrossRef - Application of High-Performance Liquid Chromatography Combined with Fluorescence Detector and Dispersive Liquid–Liquid Microextraction to Quantification of Selected Bisphenols in Human Amniotic Fluid Samples
Szymon Szubartowski, Tomasz Tuzimski
International Journal of Environmental Research and Public Health.2022; 20(1): 297. CrossRef - The Association between Phenols and Thyroid Hormones: The Role of Iodothyronine Deiodinase Genes
Blanca Sarzo, Reem Abumallouh, Natalia Marin, Sabrina Llop, Andrea Beneito, Inmaculada Lopez-Flores, Nerea Ferrero, Amrit Kaur Sakhi, ferran ballester, Maria-Jose Lopez-Espinosa
SSRN Electronic Journal .2022;[Epub] CrossRef - Bisphenols emerging in Norwegian and Czech aquatic environments show transthyretin binding potency and other less-studied endocrine-disrupting activities
Pavel Šauer, Helena Švecová, Kateřina Grabicová, Farah Gönül Aydın, Tomáš Mackuľak, Vít Kodeš, Line Diana Blytt, Liv Bruås Henninge, Roman Grabic, Hana Kocour Kroupová
Science of The Total Environment.2021; 751: 141801. CrossRef - Endocrine Disrupting Chemicals and Thyroid Cancer: An Overview
Mathilda Alsen, Catherine Sinclair, Peter Cooke, Kimia Ziadkhanpour, Eric Genden, Maaike van Gerwen
Toxics.2021; 9(1): 14. CrossRef - Thyroid-Modulating Activities of Olive and Its Polyphenols: A Systematic Review
Kok-Lun Pang, Johanna Nathania Lumintang, Kok-Yong Chin
Nutrients.2021; 13(2): 529. CrossRef - Human biomonitoring of bisphenol A along pregnancy: An exposure reconstruction of the EXHES-Spain cohort
María Ángeles Martínez, Neus González, Anna Martí, Montse Marquès, Joaquim Rovira, Vikas Kumar, Martí Nadal
Environmental Research.2021; 196: 110941. CrossRef - Dietary Intake of Endocrine Disrupting Substances Presents in Environment and Their Impact on Thyroid Function
Aneta Sokal, Sara Jarmakiewicz-Czaja, Jacek Tabarkiewicz, Rafał Filip
Nutrients.2021; 13(3): 867. CrossRef - BPA and BPA alternatives BPS, BPAF, and TMBPF, induce cytotoxicity and apoptosis in rat and human stem cells
Kristen G. Harnett, Ashley Chin, Sonya M. Schuh
Ecotoxicology and Environmental Safety.2021; 216: 112210. CrossRef - Bisphenols and the Development of Type 2 Diabetes: The Role of the Skeletal Muscle and Adipose Tissue
Fozia Ahmed, Maria Pereira, Céline Aguer
Environments.2021; 8(4): 35. CrossRef - Involvement of Thyroid Hormones in Brain Development and Cancer
Gabriella Schiera, Carlo Maria Di Liegro, Italia Di Liegro
Cancers.2021; 13(11): 2693. CrossRef - Environmental Factors Affecting Thyroid-Stimulating Hormone and Thyroid Hormone Levels
Mirjana Babić Leko, Ivana Gunjača, Nikolina Pleić, Tatijana Zemunik
International Journal of Molecular Sciences.2021; 22(12): 6521. CrossRef - Thyroid health in big city realities
Liudmila L. Kamynina
City Healthcare.2021; 2(2): 84. CrossRef - Adverse effects of bisphenol B exposure on the thyroid and nervous system in early life stages of zebrafish
Qian Yang, Zhenzhu Zhu, Qin Liu, Lihong Chen
Comparative Biochemistry and Physiology Part C: Toxicology & Pharmacology.2021; 250: 109167. CrossRef - Teratogenicity and toxicity of the new BPA alternative TMBPF, and BPA, BPS, and BPAF in chick embryonic development
Kristen G. Harnett, Lucy G. Moore, Ashley Chin, Isabel C. Cohen, Rylee R. Lautrup, Sonya M. Schuh
Current Research in Toxicology.2021; 2: 399. CrossRef - A Review on the Occurrence, Exposure, and Health Impacts of Bisphenol A
Prince Sharma, Khushboo Sharma, Geetika Sharma, Pooja Chadha
Toxicology International.2021; : 337. CrossRef - Thyroxine-binding globulin, peripheral deiodinase activity, and thyroid autoantibody status in association of phthalates and phenolic compounds with thyroid hormones in adult population
Sohyeon Choi, Min Joo Kim, Young Joo Park, Sunmi Kim, Kyungho Choi, Gi Jeong Cheon, Yoon Hee Cho, Hye Li Jeon, Jiyoung Yoo, Jeongim Park
Environment International.2020; 140: 105783. CrossRef - Clinical expression of endocrine disruptors in children
Lorenzo Iughetti, Laura Lucaccioni, Maria E. Street, Sergio Bernasconi
Current Opinion in Pediatrics.2020; 32(4): 554. CrossRef - Combined effects of di (2-ethylhexyl) phthalate and bisphenol A on thyroid hormone homeostasis in adolescent female rats
Xuan Zhang, Yuejiao Zhao, Cheng Cheng, Liuli Li, Mingyang Xiao, Guopei Zhang, Xiaobo Lu
Environmental Science and Pollution Research.2020; 27(32): 40882. CrossRef - How microplastic components influence the immune system and impact on children health: Focus on cancer
Mariana Segovia‐Mendoza, Karen E. Nava‐Castro, Margarita I. Palacios‐Arreola, Claudia Garay‐Canales, Jorge Morales‐Montor
Birth Defects Research.2020; 112(17): 1341. CrossRef - Perinatal exposure to Bisphenol A disturbs the early differentiation of male germ cells
Romina Pagotto, Clarisa G. Santamaría, María Belén Harreguy, Julián Abud, María Laura Zenclussen, Laura Kass, Martina Crispo, Mónica M. Muñoz-de-Toro, Horacio A. Rodriguez, Mariela Bollati-Fogolín
Reproductive Toxicology.2020; 98: 117. CrossRef - Novel Biobased Furanic Diols as Potential Alternatives to BPA: Synthesis and Endocrine Activity Screening
Catherine A. Sutton, Alexander Polykarpov, Keimpe Jan van den Berg, Alexander Yahkind, Linda J. Lea, Dean C. Webster, Mukund P. Sibi
ACS Sustainable Chemistry & Engineering.2020; 8(51): 18824. CrossRef
- The Role of Endocrine Disruptors Bisphenols and Phthalates in Obesity: Current Evidence, Perspectives and Controversies

- Clinical Study
- Postoperative Thyroid-Stimulating Hormone Levels Did Not Affect Recurrence after Thyroid Lobectomy in Patients with Papillary Thyroid Cancer
- Myung-Chul Lee, Min Joo Kim, Hoon Sung Choi, Sun Wook Cho, Guk Haeng Lee, Young Joo Park, Do Joon Park
- Endocrinol Metab. 2019;34(2):150-157. Published online May 10, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.2.150
- 6,701 View
- 137 Download
- 28 Web of Science
- 31 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background Thyroid-stimulating hormone (TSH) suppression is recommended for patients who undergo thyroidectomy for differentiated thyroid cancer (DTC). However, the impact of TSH suppression on clinical outcomes in low-risk DTC remains uncertain. Therefore, we investigated the effects of postoperative TSH levels on recurrence in patients with low-risk DTC after thyroid lobectomy.
Methods Patients (
n =1,528) who underwent thyroid lobectomy for papillary thyroid carcinoma between 2000 and 2012 were included in this study. According to the mean and dominant TSH values during the entire follow-up period or 5 years, patients were divided into four groups (<0.5, 0.5 to 1.9, 2.0 to 4.4, and ≥4.5 mIU/L). Recurrence-free survival was compared among the groups.Results During the 5.6 years of follow-up, 21 patients (1.4%) experienced recurrence. Mean TSH levels were within the recommended low-normal range (0.5 to 1.9 mIU/L) during the total follow-up period or 5 years in 38.1% or 36.0% of patients. The mean and dominant TSH values did not affect recurrence-free survival. Adjustment for other risk factors did not alter the results.
Conclusion Serum TSH levels did not affect short-term recurrence in patients with low-risk DTC after thyroid lobectomy. TSH suppression should be conducted more selectively.
-
Citations
Citations to this article as recorded by- Dynamic risk assessment in patients with differentiated thyroid cancer
Erika Abelleira, Fernando Jerkovich
Reviews in Endocrine and Metabolic Disorders.2024; 25(1): 79. CrossRef - Stimulating thyroglobulin to TSH ratio predict long-term efficacy of 131I therapy in patients with differentiated thyroid cancer after total thyroidectomy: a retrospective study
Xue Yin, Chao Lu, Danyang Sun, Yanhui Ji, Yan Wang, Hongyuan Zheng, Ziyu Ma, Qiang Jia, Jian Tan, Wei Zheng
Endocrine.2024;[Epub] CrossRef - Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)
Ja Kyung Lee, Eu Jeong Ku, Su-jin Kim, Woochul Kim, Jae Won Cho, Kyong Yeun Jung, Hyeong Won Yu, Yea Eun Kang, Mijin Kim, Hee Kyung Kim, Junsun Ryu, June Young Choi
Annals of Surgical Treatment and Research.2024; 106(1): 19. CrossRef - Impact of a mobile health intervention based on multi-theory model of health behavior change on self-management in patients with differentiated thyroid cancer: protocol for a randomized controlled trial
Yang Jiang, Xiangju Sun, Maomin Jiang, Hewei Min, Jing Wang, Xinghua Fu, Jiale Qi, Zhenjie Yu, Xiaomei Zhu, Yibo Wu
Frontiers in Public Health.2024;[Epub] CrossRef - Risk of Subsequent Primary Cancers in Thyroid Cancer Survivors according to the Dose of Levothyroxine: A Nationwide Cohort Study
Min-Su Kim, Jang Won Lee, Min Kyung Hyun, Young Shin Song
Endocrinology and Metabolism.2024; 39(2): 288. CrossRef - Outcomes and Trends of Treatments in High‐Risk Differentiated Thyroid Cancer
Arash Abiri, Khodayar Goshtasbi, Sina J. Torabi, Edward C. Kuan, William B. Armstrong, Tjoson Tjoa, Yarah M. Haidar
Otolaryngology–Head and Neck Surgery.2023; 168(4): 745. CrossRef - Outcomes of Patients with an Intermediate‐Risk Group According to the Japanese Risk Classification of Papillary Thyroid Carcinoma
Kiyomi Horiuchi, Mikiko Fujimoto, Kamio Hidenori, Yusaku Yoshida, Eiichiro Noguchi, Yoko Omi, Takahiro Okamoto
World Journal of Surgery.2023; 47(10): 2464. CrossRef - Effects of Isthmus Preservation on Postoperative Hypothyroidism after Lobectomy
Yeong San Jeon, Wan Wook Kim
International Journal of Thyroidology.2023; 16(1): 120. CrossRef - Physical activity and reduced risk of fracture in thyroid cancer patients after thyroidectomy — a nationwide cohort study
Jinyoung Kim, Kyungdo Han, Jin-Hyung Jung, Jeonghoon Ha, Chaiho Jeong, Jun-Young Heu, Se-Won Lee, Jeongmin Lee, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Ki-Ho Song, Ki-Hyun Baek
Frontiers in Endocrinology.2023;[Epub] CrossRef - Association between thyroid stimulating hormone levels and papillary thyroid cancer risk: A meta-analysis
Bin Xu, Shu-Yan Gu, Ning-Ming Zhou, Jun-Jie Jiang
Open Life Sciences.2023;[Epub] CrossRef - The Relationship between Thyrotropin Serum Concentrations and Thyroid Carcinoma
Xueqi Zhang, Lijun Tian, Di Teng, Weiping Teng
Cancers.2023; 15(20): 5017. CrossRef - Differentiated thyroid cancer: a focus on post-operative thyroid hormone replacement and thyrotropin suppression therapy
Benjamin J. Gigliotti, Sina Jasim
Endocrine.2023; 83(2): 251. CrossRef - Optimal Serum Thyrotropin Level for Patients with Papillary Thyroid Carcinoma After Lobectomy
Siyuan Xu, Ying Huang, Hui Huang, Xiaohang Zhang, Jiaxin Qian, Xiaolei Wang, Zhengang Xu, Shaoyan Liu, Jie Liu
Thyroid.2022; 32(2): 138. CrossRef - Optimal Thyrotropin Following Lobectomy for Papillary Thyroid Cancer: Does It Exist?
Lindsay Bischoff, Megan R. Haymart
Thyroid.2022; 32(2): 117. CrossRef - Evaluation of ITGA3 as a Biomarker of Progression and Recurrence in Papillary Thyroid Carcinoma
Guoliang Zhang, Bing Li, Yuanmei Lin
Frontiers in Oncology.2022;[Epub] CrossRef - The Question of an Optimal TSH Goal After Lobectomy for Papillary Thyroid Cancer
Bernadette Biondi
Clinical Thyroidology.2022; 34(2): 67. CrossRef - Is Maintaining Thyroid-Stimulating Hormone Effective in Patients Undergoing Thyroid Lobectomy for Low-Risk Differentiated Thyroid Cancer? A Systematic Review and Meta-Analysis
Ho-Ryun Won, Eonju Jeon, Jae Won Chang, Yea Eun Kang, Kunho Song, Sun Wook Kim, Dong Mee Lim, Tae Kwun Ha, Ki-Wook Chung, Hyo-Jeong Kim, Young Joo Park, Bon Seok Koo
Cancers.2022; 14(6): 1470. CrossRef - Research Review of Thermal Ablation in the Treatment of Papillary Thyroid Carcinoma
Di Ou, Chen Chen, Tian Jiang, Dong Xu
Frontiers in Oncology.2022;[Epub] CrossRef - CACA guidelines for holistic integrative management of thyroid cancer
Minghua Ge, Ming Gao, Ruochuan Cheng, Xiaohong Chen, Haixia Guan, Yansong Lin, Shaoyan Liu, Yu Wang, Chuanming Zheng, Xiangqian Zheng
Holistic Integrative Oncology.2022;[Epub] CrossRef - Value of thyroglobulin post hemithyroidectomy for cancer: a literature review
Saam S. Tourani, Bill Fleming, Justin Gundara
ANZ Journal of Surgery.2021; 91(4): 724. CrossRef - Pros and cons of hemi‐thyroidectomy for low‐risk differentiated thyroid cancer
Alexander J. Papachristos, Anthony Glover, Mark S. Sywak, Stan B. Sidhu
ANZ Journal of Surgery.2021; 91(9): 1704. CrossRef - Management and follow-up of differentiated thyroid cancer not submitted to radioiodine treatment: a systematic review
Carla GAMBALE, Rossella ELISEI, Antonio MATRONE
Minerva Endocrinologica.2021;[Epub] CrossRef - The Recovery of Thyroid Function in Low-Risk Papillary Thyroid Cancer After Lobectomy: A 3-Year Follow-Up Study
Yi Dou, Yingji Chen, Daixing Hu, Xinliang Su
Frontiers in Endocrinology.2021;[Epub] CrossRef - Controversy: For or against thyroid lobectomy in > 1 cm differentiated thyroid cancer?
Fabrice Menegaux, Jean-Christophe Lifante
Annales d'Endocrinologie.2021; 82(2): 78. CrossRef - Thyroid cancer, recent advances in diagnosis and therapy
Fadi Nabhan, Priya H. Dedhia, Matthew D. Ringel
International Journal of Cancer.2021; 149(5): 984. CrossRef - A Multicenter, Randomized, Controlled Trial for Assessing the Usefulness of Suppressing Thyroid Stimulating Hormone Target Levels after Thyroid Lobectomy in Low to Intermediate Risk Thyroid Cancer Patients (MASTER): A Study Protocol
Eun Kyung Lee, Yea Eun Kang, Young Joo Park, Bon Seok Koo, Ki-Wook Chung, Eu Jeong Ku, Ho-Ryun Won, Won Sang Yoo, Eonju Jeon, Se Hyun Paek, Yong Sang Lee, Dong Mee Lim, Yong Joon Suh, Ha Kyoung Park, Hyo-Jeong Kim, Bo Hyun Kim, Mijin Kim, Sun Wook Kim, Ka
Endocrinology and Metabolism.2021; 36(3): 574. CrossRef - Long-term follow-up results of PTMC treated by ultrasound-guided radiofrequency ablation: a retrospective study
Yalin Zhu, Ying Che, Shuhang Gao, Shuangsong Ren, Mengying Tong, Lina Wang, Fang Yang
International Journal of Hyperthermia.2021; 38(1): 1225. CrossRef - Thyroid Hormone Supplementation Therapy for Differentiated Thyroid Cancer After Lobectomy: 5 Years of Follow-Up
Soo Young Kim, Hee Jun Kim, Seok-Mo Kim, Hojin Chang, Yong Sang Lee, Hang-Seok Chang, Cheong Soo Park
Frontiers in Endocrinology.2020;[Epub] CrossRef - Thyroid Lobectomy for Low to Intermediate Risk Differentiated Thyroid Cancer
Dana M. Hartl, Joanne Guerlain, Ingrid Breuskin, Julien Hadoux, Eric Baudin, Abir Al Ghuzlan, Marie Terroir-Cassou-Mounat, Livia Lamartina, Sophie Leboulleux
Cancers.2020; 12(11): 3282. CrossRef - Annual Neck Ultrasonography Surveillance between 3 to 12 Years after Thyroid Lobectomy for Papillary Thyroid Microcarcinoma
Jin Gu Kang, Jung Eun Choi, Soo Jung Lee, Su Hwan Kang
International Journal of Thyroidology.2020; 13(2): 142. CrossRef - Thyroid hormone therapy in differentiated thyroid cancer
Giorgio Grani, Valeria Ramundo, Antonella Verrienti, Marialuisa Sponziello, Cosimo Durante
Endocrine.2019; 66(1): 43. CrossRef
- Dynamic risk assessment in patients with differentiated thyroid cancer

- Miscellaneous
- Corrigendum: Author's Name Correction. Study Protocol of Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma (MAeSTro)
- Jae Hoon Moon, Ji-hoon Kim, Eun Kyung Lee, Kyu Eun Lee, Sung Hye Kong, Yeo Koon Kim, Woo-Jin Jeong, Chang Yoon Lee, Roh-Eul Yoo, Yul Hwangbo, Young Shin Song, Min Joo Kim, Sun Wook Cho, Su-jin Kim, Eun-Jae Chung, June Young Choi, Chang Hwan Ryu, You Jin Lee, Jeong Hun Hah, Yuh-Seog Jung, Junsun Ryu, Yunji Hwang, Sue K. Park, Ho Kyung Sung, Ka Hee Yi, Do Joon Park, Young Joo Park
- Endocrinol Metab. 2018;33(3):427. Published online August 14, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.3.427
- 3,505 View
- 48 Download
- 2 Web of Science
- 2 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Invasiveness and Metastatic Aggressiveness in Small Differentiated Thyroid Cancers: Demography of Small Papillary Thyroid Carcinomas in the Swedish Population
Haytham Bayadsi, Martin Bergman, Malin Sund, Joakim Hennings
World Journal of Surgery.2020; 44(2): 461. CrossRef - Clinical and pathologic predictors of lymph node metastasis in papillary thyroid microcarcinomas
Ling Zhao, Xiaoya Sun, Yukun Luo, Fulin Wang, Zhaohui Lyu
Annals of Diagnostic Pathology.2020; 49: 151647. CrossRef
- Invasiveness and Metastatic Aggressiveness in Small Differentiated Thyroid Cancers: Demography of Small Papillary Thyroid Carcinomas in the Swedish Population

- Thyroid
- Study Protocol of Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma (MAeSTro)
- Jae Hoon Moon, Ji-hoon Kim, Eun Kyung Lee, Kyu Eun Lee, Sung Hye Kong, Yeo Koon Kim, Woo-jin Jung, Chang Yoon Lee, Roh-Eul Yoo, Yul Hwangbo, Young Shin Song, Min Joo Kim, Sun Wook Cho, Su-jin Kim, Eun Jae Jung, June Young Choi, Chang Hwan Ryu, You Jin Lee, Jeong Hun Hah, Yuh-Seog Jung, Junsun Ryu, Yunji Hwang, Sue K. Park, Ho Kyung Sung, Ka Hee Yi, Do Joon Park, Young Joo Park
- Endocrinol Metab. 2018;33(2):278-286. Published online June 21, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.2.278
- 5,440 View
- 88 Download
- 34 Web of Science
- 32 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background The ongoing Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma (MAeSTro) aims to observe the natural course of papillary thyroid microcarcinoma (PTMC), develop a protocol for active surveillance (AS), and compare the long-term prognosis, quality of life, and medical costs between the AS and immediate surgery groups.
Methods This multicenter prospective cohort study of PTMC started in June 2016. The inclusion criteria were suspicious of malignancy or malignancy based on fine needle aspiration or core needle biopsy, age of ≥18 years, and a maximum diameter of ≤1 cm. If there was no major organ involvement, no lymph node/distant metastasis, and no variants with poor prognosis, the patients were explained of the pros and cons of immediate surgery and AS before selecting AS or immediate surgery. Follow-up visits (physical examination, ultrasonography, thyroid function, and questionnaires) are scheduled every 6 months during the first 2 years, and then every 1 year thereafter. Progression was defined as a maximum diameter increase of ≥3, ≥2 mm in two dimensions, suspected organ involvement, or lymph node/distant metastasis.
Results Among 439 enrolled patients, 290 patients (66.1%) chose AS and 149 patients (33.9%) chose immediate surgery. The median follow-up was 6.7 months (range, 0.2 to 11.9). The immediate surgery group had a larger maximum tumor diameter, compared to the AS group (7.1±1.9 mm vs. 6.6±2.0 mm, respectively;
P =0.014).Conclusion The results will be useful for developing an appropriate PTMC treatment policy based on its natural course and risk factors for progression.
-
Citations
Citations to this article as recorded by- 2023 Update of the Korean Thyroid Association Guidelines for the Management of Thyroid Nodules
Eun Kyung Lee, Young Joo Park
Clinical Thyroidology®.2024; 36(4): 153. CrossRef - Psychological adjustment to initial treatment for low‐risk thyroid cancer: Preliminary study
Gabriella T. Seo, Mark L. Urken, Lauren E. Wein, Michael P. Saturno, Danielle Kapustin, Monica H. Xing, Lauren E. Yue, Eric M. Dowling, Tracey A. Revenson, Katherine J. Roberts, Robert Michael Tuttle
Head & Neck.2023; 45(2): 439. CrossRef - Response to Letter to the Editor on Surgical Outcomes in Patients With Low-Risk Papillary Thyroid Microcarcinoma From MAeSTro Study: Immediate Operation Versus Delayed Operation Following Active Surveillance: A Multicenter Prospective Cohort Study
Hyeonuk Hwang, June Young Choi, Jae Hoon Moon, Eun Kyung Lee, Young Joo Park, Su-jin Kim, Yuh-Seog Jung
Annals of Surgery Open.2023; 4(3): e311. CrossRef - Lower Thyroid Cancer Mortality in Patients Detected by Screening: A Meta-Analysis
Shinje Moon, Young Shin Song, Kyong Yeun Jung, Eun Kyung Lee, Young Joo Park
Endocrinology and Metabolism.2023; 38(1): 93. CrossRef - To Screen or Not to Screen?
Do Joon Park
Endocrinology and Metabolism.2023; 38(1): 69. CrossRef - Surgical Outcomes in Patients With Low-risk Papillary Thyroid Microcarcinoma From MAeSTro Study
Hyeonuk Hwang, June Young Choi, Hyeong Won Yu, Jae Hoon Moon, Ji-hoon Kim, Eun Kyung Lee, Yeo Koon Kim, Chang Yoon Lee, Sun Wook Cho, Eun-Jae Chung, Chang Hwan Ryu, Junsun Ryu, Ka Hee Yi, Do Joon Park, Kyu Eun Lee, Young Joo Park, Su-jin Kim, Yuh-Seog Jun
Annals of Surgery.2023; 278(5): e1087. CrossRef - US Predictors of Papillary Thyroid Microcarcinoma Progression at Active Surveillance
Ji Ye Lee, Ji-hoon Kim, Yeo Koon Kim, Chang Yoon Lee, Eun Kyung Lee, Jae Hoon Moon, Hoon Sung Choi, Hwangbo Yul, Sun Wook Cho, Su-jin Kim, Kyu Eun Lee, Do Joon Park, Young Joo Park
Radiology.2023;[Epub] CrossRef - MET-receptor targeted fluorescent imaging and spectroscopy to detect multifocal papillary thyroid cancer
Madelon J. H. Metman, Pascal K. C. Jonker, Luc H. J. Sondorp, Bettien M. van Hemel, Mark S. Sywak, Anthony J. Gill, Liesbeth Jansen, Paul J. van Diest, Tessa M. van Ginhoven, Clemens W. G. M. Löwik, Anh H. Nguyen, Dominic J. Robinson, Gooitzen M. van Dam,
European Journal of Nuclear Medicine and Molecular Imaging.2023;[Epub] CrossRef - Active Surveillance of Thyroid Microcarcinomas: a Critical View
Claudio R. Cernea, Leandro Luongo Matos, Cecília Eugênio, Giovanna Mattos Ferreira, Yasmin Sa Cerqueira, Ana Kober N. Leite, Felipe A. B. Vanderlei, Dorival de Carlucci, Renato N. Gotoda, Flávio C. Hojaij, Vergilius J. F. Araújo-Filho
Current Oncology Reports.2022; 24(1): 69. CrossRef - Active Surveillance Versus Thyroid Surgery for Differentiated Thyroid Cancer: A Systematic Review
Roger Chou, Tracy Dana, Megan Haymart, Angela M. Leung, Ralph P. Tufano, Julie Ann Sosa, Matthew D. Ringel
Thyroid.2022; 32(4): 351. CrossRef - A Review of Active Surveillance of Papillary Thyroid Microcarcinoma
Cho Rok Lee
Journal of Endocrine Surgery.2022; 22(1): 1. CrossRef - Active Surveillance Versus Immediate Surgery for Low-Risk Papillary Thyroid Microcarcinoma Patients in South Korea: A Cost-Minimization Analysis from the MAeSTro Study
Kyungsik Kim, June Young Choi, Su-jin Kim, Eun Kyung Lee, Young Ki Lee, Jun Sun Ryu, Kyu Eun Lee, Jae Hoon Moon, Young Joo Park, Sun Wook Cho, Sue K. Park
Thyroid.2022; 32(6): 648. CrossRef - A cross-sectional survey of patient treatment choice in a multicenter prospective cohort study on active surveillance of papillary thyroid microcarcinoma (MAeSTro)
Yul Hwangbo, June Young Choi, Eun Kyung Lee, Chang Hwan Ryu, Sun Wook Cho, Eun Jae Chung, Jeong Hun Hah, Woo-Jin Jeong, Sue K. Park, Yuh-Seog Jung, Ji-hoon Kim, Min Joo Kim, Su-jin Kim, Yeo Koon Kim, Chang Yoon Lee, Ji Ye Lee, You Jin Lee, Hyeong Won Yu,
Thyroid.2022;[Epub] CrossRef - Progression of Low-Risk Papillary Thyroid Microcarcinoma During Active Surveillance: Interim Analysis of a Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma in Korea
Eun Kyung Lee, Jae Hoon Moon, Yul Hwangbo, Chang Hwan Ryu, Sun Wook Cho, June Young Choi, Eun-Jae Chung, Woo-Jin Jeong, Yuh-Seog Jung, Junsun Ryu, Su-jin Kim, Min Joo Kim, Yeo Koon Kim, Chang Yoon Lee, Ji Ye Lee, Hyeong Won Yu, Jeong Hun Hah, Kyu Eun Lee,
Thyroid.2022; 32(11): 1328. CrossRef - Indications and Strategy for Active Surveillance of Adult Low-Risk Papillary Thyroid Microcarcinoma: Consensus Statements from the Japan Association of Endocrine Surgery Task Force on Management for Papillary Thyroid Microcarcinoma
Iwao Sugitani, Yasuhiro Ito, Dai Takeuchi, Hirotaka Nakayama, Chie Masaki, Hisakazu Shindo, Masanori Teshima, Kazuhiko Horiguchi, Yusaku Yoshida, Toshiharu Kanai, Mitsuyoshi Hirokawa, Kiyomi Y. Hames, Isao Tabei, Akira Miyauchi
Thyroid.2021; 31(2): 183. CrossRef - Effect of Initial Treatment Choice on 2-year Quality of Life in Patients with Low-risk Papillary Thyroid Microcarcinoma
Jae Hoon Moon, Chang Hwan Ryu, Sun Wook Cho, June Young Choi, Eun-Jae Chung, Jeong Hun Hah, Yul Hwangbo, Woo-Jin Jeong, Yuh-Seog Jung, Ji-hoon Kim, Min Joo Kim, Su-jin Kim, Yeo Koon Kim, Chang Yoon Lee, Eun Kyung Lee, Ji Ye Lee, Kyu Eun Lee, You Jin Lee,
The Journal of Clinical Endocrinology & Metabolism.2021; 106(3): 724. CrossRef - Adoption of Active Surveillance for Very Low-Risk Differentiated Thyroid Cancer in the United States: A National Survey
Susan C Pitt, Nan Yang, Megan C Saucke, Nicholas Marka, Bret Hanlon, Kristin L Long, Alexandria D McDow, J P Brito, Benjamin R Roman
The Journal of Clinical Endocrinology & Metabolism.2021; 106(4): 1728. CrossRef - Protocol for a Korean Multicenter Prospective Cohort Study of Active Surveillance or Surgery (KoMPASS) in Papillary Thyroid Microcarcinoma
Min Ji Jeon, Yea Eun Kang, Jae Hoon Moon, Dong Jun Lim, Chang Yoon Lee, Yong Sang Lee, Sun Wook Kim, Min-Hee Kim, Bo Hyun Kim, Ho-Cheol Kang, Minho Shong, Sun Wook Cho, Won Bae Kim
Endocrinology and Metabolism.2021; 36(2): 359. CrossRef - Multifocality and Progression of Papillary Thyroid Microcarcinoma During Active Surveillance
Ryuta Nagaoka, Aya Ebina, Kazuhisa Toda, Tomoo Jikuzono, Marie Saitou, Masaomi Sen, Hiroko Kazusaka, Mami Matsui, Keiko Yamada, Hiroki Mitani, Iwao Sugitani
World Journal of Surgery.2021; 45(9): 2769. CrossRef - Active Surveillance as an Effective Management Option for Low-Risk Papillary Thyroid Microcarcinoma
Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Endocrinology and Metabolism.2021; 36(4): 717. CrossRef - The Concept of Economic Evaluation and Its Application in Thyroid Cancer Research
Kyungsik Kim, Mijin Kim, Woojin Lim, Bo Hyun Kim, Sue K. Park
Endocrinology and Metabolism.2021; 36(4): 725. CrossRef - Genomic and Transcriptomic Characteristics According to Size of Papillary Thyroid Microcarcinoma
Young Shin Song, Byung-Hee Kang, Seungbok Lee, Seong-Keun Yoo, Young Sik Choi, Jungsun Park, Dong Yoon Park, Kyu Eun Lee, Jeong-Sun Seo, Young Joo Park
Cancers.2020; 12(5): 1345. CrossRef - Experience with Active Surveillance of Thyroid Low-Risk Carcinoma in a Developing Country
Alvaro Sanabria
Thyroid.2020; 30(7): 985. CrossRef - Association of Patient Age With Progression of Low-risk Papillary Thyroid Carcinoma Under Active Surveillance
Alexandra Koshkina, Rouhi Fazelzad, Iwao Sugitani, Akira Miyauchi, Lehana Thabane, David P. Goldstein, Sangeet Ghai, Anna M. Sawka
JAMA Otolaryngology–Head & Neck Surgery.2020; 146(6): 552. CrossRef - Active surveillance in low risk papillary thyroid carcinoma
Fabian Pitoia, Anabella Smulever
World Journal of Clinical Oncology.2020; 11(6): 320. CrossRef - Early Diagnosis of Low-Risk Papillary Thyroid Cancer Results Rather in Overtreatment Than a Better Survival
Jolanta Krajewska, Aleksandra Kukulska, Malgorzata Oczko-Wojciechowska, Agnieszka Kotecka-Blicharz, Katarzyna Drosik-Rutowicz, Malgorzata Haras-Gil, Barbara Jarzab, Daria Handkiewicz-Junak
Frontiers in Endocrinology.2020;[Epub] CrossRef - The dilemma of papillary thyroid microcarcinoma management. To operate or not to operate, that is the question
Juan C Galofré
Endocrinología, Diabetes y Nutrición.2019; 66(8): 469. CrossRef - Computed Tomography for Detecting Cervical Lymph Node Metastasis in Patients Who Have Papillary Thyroid Microcarcinoma with Tumor Characteristics Appropriate for Active Surveillance
Dong-Hwa Lee, Yeo Koon Kim, Hyeong Won Yu, June Young Choi, So Yeon Park, Jae Hoon Moon
Thyroid.2019; 29(11): 1653. CrossRef - The dilemma of papillary thyroid microcarcinoma management. To operate or not to operate, that is the question
Juan C Galofré
Endocrinología, Diabetes y Nutrición (English ed.).2019; 66(8): 469. CrossRef - Longitudinal Assessment of Quality of Life According to Treatment Options in Low-Risk Papillary Thyroid Microcarcinoma Patients: Active Surveillance or Immediate Surgery (Interim Analysis of MAeSTro)
Sung Hye Kong, Junsun Ryu, Min Joo Kim, Sun Wook Cho, Young Shin Song, Ka Hee Yi, Do Joon Park, Yul Hwangbo, You Jin Lee, Kyu Eun Lee, Su-jin Kim, Woo-Jin Jeong, Eun-Jae Chung, Jeong Hun Hah, June Young Choi, Chang Hwan Ryu, Yuh-Seog Jung, Jae Hoon Moon,
Thyroid.2019; 29(8): 1089. CrossRef - Ultrasound-guided percutaneous laser ablation for papillary thyroid microcarcinoma: a retrospective analysis of 37 patients
Lili Ji, Qin Wu, Jun Gu, Xuedong Deng, Wei Zhou, Xing Fan, Feng Zhou
Cancer Imaging.2019;[Epub] CrossRef - Evolving management considerations in active surveillance for micropapillary thyroid carcinoma
Allen S. Ho, Irene Chen, Michelle Melany, Wendy L. Sacks
Current Opinion in Endocrinology, Diabetes & Obesity.2018; 25(5): 353. CrossRef
- 2023 Update of the Korean Thyroid Association Guidelines for the Management of Thyroid Nodules

- Thyroid
- Star-Shaped Intense Uptake of 131I on Whole Body Scans Can Reflect Good Therapeutic Effects of Low-Dose Radioactive Iodine Treatment of 1.1 GBq
- Sung Hye Kong, Jung Ah Lim, Young Shin Song, Shinje Moon, Ye An Kim, Min Joo Kim, Sun Wook Cho, Jae Hoon Moon, Ka Hee Yi, Do Joon Park, Bo Youn Cho, Young Joo Park
- Endocrinol Metab. 2018;33(2):228-235. Published online May 4, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.2.228
- 5,302 View
- 50 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background After initial radioactive iodine (RAI) treatment in differentiated thyroid cancer patients, we sometimes observe a star-shaped region of intense uptake of 131I on whole body scans (WBSs), called a ‘star artifact.’ We evaluated the clinical implications of star artifacts on the success rate of remnant ablation and long-term prognosis.
Methods Total 636 patients who received 131I dose of 1.1 GBq for the initial RAI therapy and who did not show distant metastasis at the time of diagnosis were retrospectively evaluated. A negative second WBS was used for evaluating the ablation efficacy of the RAI therapy. Among them, 235 patients (36.9%) showed a star artifact on their first WBS.
Results In patients with first stimulated thyroglobulin (sTg) levels ≤2 ng/mL, patients with star artifacts had a higher rate of negative second WBS compared with those without star artifacts (77.8% vs. 63.9%,
P =0.044), and showed significantly higher recurrence-free survival (P =0.043) during the median 8.0 years (range, 1.0 to 10.0) of follow-up. The 5- and 10-year recurrence rates (5YRR, 10YRR) were also significantly lower in patients with star artifacts compared with those without (0% vs. 4.9%, respectively,P =0.006 for 5YRR; 0% vs. 6.4%, respectively,P =0.005 for 10YRR). However, ablation success rate or recurrence-free survival was not different among patients whose first sTg levels >2 ng/mL regardless of star artifacts.Conclusion Therefore, star artifacts at initial RAI therapy imply a good ablation efficacy or a favorable long-term prognosis in patients with sTg levels ≤2 ng/mL.
-
Citations
Citations to this article as recorded by- Prognostic value of star-shaped intense uptake of 131I in thyroid cancer patients
Liu Xiao, Wen Jie Zhang, Yue Qi Wang, Lin Li
Revista Española de Medicina Nuclear e Imagen Molecular (English Edition).2021; 40(1): 30. CrossRef - Valores pronósticos de la captación en estrella de 131I en pacientes con cáncer diferenciado de tiroides
L. Xiao, W.J. Zhang, Y.Q. Wang, L. Li
Revista Española de Medicina Nuclear e Imagen Molecular.2021; 40(1): 30. CrossRef - Comparison between planar and single-photon computed tomography images for radiation intensity quantification in iodine-131 scintigraphy
Yusuke Iizuka, Tomohiro Katagiri, Minoru Inoue, Kiyonao Nakamura, Takashi Mizowaki
Scientific Reports.2021;[Epub] CrossRef
- Prognostic value of star-shaped intense uptake of 131I in thyroid cancer patients

- Obesity and Metabolism
- Mitochondrial Complexes I and II Are More Susceptible to Autophagy Deficiency in Mouse β-Cells
- Min Joo Kim, Ok Kyong Choi, Kyung Sil Chae, Min Kyeong Kim, Jung Hee Kim, Masaaki Komatsu, Keiji Tanaka, Hakmo Lee, Sung Soo Chung, Soo Heon Kwak, Young Min Cho, Kyong Soo Park, Hye Seung Jung
- Endocrinol Metab. 2015;30(1):65-70. Published online March 27, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.1.65
- 3,957 View
- 40 Download
- 4 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Damaged mitochondria are removed by autophagy. Therefore, impairment of autophagy induces the accumulation of damaged mitochondria and mitochondrial dysfunction in most mammalian cells. Here, we investigated mitochondrial function and the expression of mitochondrial complexes in autophagy-related 7 (
Atg7 )-deficient β-cells.Methods To evaluate the effect of autophagy deficiency on mitochondrial function in pancreatic β-cells, we isolated islets from
Atg7 F/F:RIP-Cre + mice and wild-type littermates. Oxygen consumption rate and intracellular adenosine 5'-triphosphate (ATP) content were measured. The expression of mitochondrial complex genes inAtg7 -deficient islets and in β-TC6 cells transfected with siAtg7 was measured by quantitative real-time polymerase chain reaction.Results Baseline oxygen consumption rate of
Atg7 -deficient islets was significantly lower than that of control islets (P <0.05). Intracellular ATP content ofAtg7 -deficient islets during glucose stimulation was also significantly lower than that of control islets (P <0.05). By Oxygraph-2k analysis, mitochondrial respiration inAtg7 -deficient islets was significantly decreased overall, although state 3 respiration and responses to antimycin A were unaffected. The mRNA levels of mitochondrial complexes I, II, III, and V inAtg7 -deficient islets were significantly lower than in control islets (P <0.05). Down-regulation ofAtg7 in β-TC6 cells also reduced the expression of complexes I and II, with marginal significance (P <0.1).Conclusion Impairment of autophagy in pancreatic β-cells suppressed the expression of some mitochondrial respiratory complexes, and may contribute to mitochondrial dysfunction. Among the complexes, I and II seem to be most vulnerable to autophagy deficiency.
-
Citations
Citations to this article as recorded by- Proteomic pathways to metabolic disease and type 2 diabetes in the pancreatic islet
Belinda Yau, Sheyda Naghiloo, Alexis Diaz-Vegas, Austin V. Carr, Julian Van Gerwen, Elise J. Needham, Dillon Jevon, Sing-Young Chen, Kyle L. Hoehn, Amanda E. Brandon, Laurence Macia, Gregory J. Cooney, Michael R. Shortreed, Lloyd M. Smith, Mark P. Keller,
iScience.2021; 24(10): 103099. CrossRef - Natural compound oblongifolin C inhibits autophagic flux, and induces apoptosis and mitochondrial dysfunction in human cholangiocarcinoma QBC939 cells
Aiqing Zhang, Wei He, Huimin Shi, Xiaodan Huang, Guozhong Ji
Molecular Medicine Reports.2016; 14(4): 3179. CrossRef - Autophagy deficiency in β cells blunts incretin-induced suppression of glucagon release from α cells
Min Joo Kim, Ok Kyong Choi, Kyung Sil Chae, Hakmo Lee, Sung Soo Chung, Dong-Sik Ham, Ji-Won Kim, Kun-Ho Yoon, Kyong Soo Park, Hye Seung Jung
Islets.2015; 7(5): e1129096. CrossRef
- Proteomic pathways to metabolic disease and type 2 diabetes in the pancreatic islet

- Preoperative Localization and Intraoperative Parathyroid Hormone Assay in Korean Patients with Primary Hyperparathyroidism
- Eirie Cho, Jung Mi Chang, Seok Young Yoon, Gil Tae Lee, Yun Hyi Ku, Hong Il Kim, Myung-Chul Lee, Guk Haeng Lee, Min Joo Kim
- Endocrinol Metab. 2014;29(4):464-469. Published online December 29, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.4.464
- 3,530 View
- 32 Download
- 8 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The intraoperative parathyroid hormone (IOPTH) assay is widely used in patients with primary hyperparathyroidism (PHPT). We investigated the usefulness of the IOPTH assay in Korean patients with PHPT.
Methods We retrospectively reviewed the data of 33 patients with PHPT who underwent parathyroidectomy. Neck ultrasonography (US) and 99mTc-sestamibi scintigraphy (MIBI scan) were performed preoperatively and IOPTH assays were conducted.
Results The sensitivity of neck US and MIBI scans were 91% and 94%, respectively. A 50% decrease in parathyroid hormone (PTH) levels 10 minutes after excision of the parathyroid gland was obtained in 91% (30/33) of patients and operative success was achieved in 97% (32/33) of patients. The IOPTH assay was 91% true-positive, 3% true-negative, 0% false-positive, and 6% false-negative. The overall accuracy of the IOPTH assay was 94%. In five cases with discordant neck US and MIBI scan results, a sufficient decrease in IOPTH levels helped the surgeon confirm the complete excision of the parathyroid gland with no additional neck exploration.
Conclusion The IOPTH assay is an accurate tool for localizing hyperfunctioning parathyroid glands and is helpful for evaluating cases with discordant neck US and MIBI scan results.
-
Citations
Citations to this article as recorded by- Single-Center Experience of Parathyroidectomy Using Intraoperative Parathyroid Hormone Monitoring
Seong Hoon Kim, Si Yeon Lee, Eun Ah Min, Young Mi Hwang, Yun Suk Choi, Jin Wook Yi
Medicina.2022; 58(10): 1464. CrossRef - The natural history and hip geometric changes of primary hyperparathyroidism without parathyroid surgery
Kyong Yeun Jung, A. Ram Hong, Dong Hwa Lee, Jung Hee Kim, Kyoung Min Kim, Chan Soo Shin, Seong Yeon Kim, Sang Wan Kim
Journal of Bone and Mineral Metabolism.2017; 35(3): 278. CrossRef - The utility of the radionuclide probe in parathyroidectomy for primary hyperparathyroidism
MS Lim, M Jinih, CH Ngai, NM Foley, HP Redmond
The Annals of The Royal College of Surgeons of England.2017; 99(5): 369. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef
- Single-Center Experience of Parathyroidectomy Using Intraoperative Parathyroid Hormone Monitoring

- Thyroid
- Medullary Thyroid Carcinoma with Ectopic Adrenocorticotropic Hormone Syndrome
- Hong Seok Choi, Min Joo Kim, Chae Ho Moon, Jong Ho Yoon, Ha Ra Ku, Geon Wook Kang, Im Il Na, Seung-Sook Lee, Byung-Chul Lee, Young Joo Park, Hong Il Kim, Yun Hyi Ku
- Endocrinol Metab. 2014;29(1):96-100. Published online March 14, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.1.96
- 3,700 View
- 40 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Ectopic adrenocorticotropic hormone (ACTH) syndrome is caused most frequently by a bronchial carcinoid tumor or by small cell lung cancer. Medullary thyroid carcinoma (MTC) is a rare etiology of ectopic ACTH syndrome. We describe a case of Cushing syndrome due to ectopic ACTH production from MTC in a 48-year-old male. He was diagnosed with MTC 14 years ago and underwent total thyroidectomy, cervical lymph node dissection and a series of metastasectomies. MTC was confirmed by the pathological examination of the thyroid and metastatic mediastinal lymph node tissues. Two years after his last surgery, he developed Cushingoid features, such as moon face and central obesity, accompanied by uncontrolled hypertension and new-onset diabetes. The laboratory results were compatible with ectopic ACTH syndrome. A bilateral adrenalectomy improved the clinical and laboratory findings that were associated with Cushing syndrome. This is the first confirmed case of ectopic ACTH syndrome caused by MTC in Korea.
-
Citations
Citations to this article as recorded by- Medullary Thyroid Cancer with Ectopic Cushing's Syndrome: A Case Report and Systematic Review of Detailed Cases from the Literature
Andrea Corsello, Vittoria Ramunno, Pietro Locantore, Giovanni Pacini, Esther Diana Rossi, Francesco Torino, Alfredo Pontecorvi, Carmela De Crea, Rosa Maria Paragliola, Marco Raffaelli, Salvatore Maria Corsello
Thyroid.2022; 32(11): 1281. CrossRef - Mucosal Neuroma Cues for Endocrine Emergency Treatment
Gyu Gang Choi, Hwan Jin Lee, Hyo Jin Han, Young Beom Jeong, Heung Bum Lee, Ji Hyun Park
Endocrinology and Metabolism.2021; 36(6): 1312. CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef - Rapid response of hypercortisolism to vandetanib treatment in a patient with advanced medullary thyroid cancer and ectopic Cushing syndrome
Fabián Pitoia, Fernanda Bueno, Angélica Schmidt, Sabrina Lucas, Graciela Cross
Archives of Endocrinology and Metabolism.2015; 59(4): 343. CrossRef
- Medullary Thyroid Cancer with Ectopic Cushing's Syndrome: A Case Report and Systematic Review of Detailed Cases from the Literature

- Characterization of Incidentally Detected Adrenal Pheochromocytoma.
- Ye An Kim, Yul Hwangbo, Min Joo Kim, Hyung Jin Choi, Je Hyun Seo, Yenna Lee, Soo Heun Kwak, Eu Jeong Ku, Tae Jung Oh, Eun Roh, Jae Hyun Bae, Jung Hee Kim, Kyoung Soo Park, Seong Yeon Kim
- Endocrinol Metab. 2012;27(2):132-137. Published online June 20, 2012
- DOI: https://doi.org/10.3803/EnM.2012.27.2.132
- 2,287 View
- 28 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
In approach to an adrenal incidentaloma, early exclusion of pheochromocytoma is clinically important, due to the risk of catecholamine crisis. The aims of this study are to investigate the characteristics of incidentally detected pheochromocytomas, compared with that of the other adrenal incidentalomas, and to compare these characteristics with those of symptomatic pheochromocytomas. METHODS: In this retrospective study, we reviewed the medical records of 198 patients with adrenal incidentaloma from 2001 to 2010. We analyzed the clinical, laboratory and radiological data of pheochromocytomas, in comparison with those of the other adrenal incidentalomas. We also compared the characteristics of these incidentally detected pheochromocytomas with the medical records of 28 pathologically proven pheochromocytomas, diagnosed based on typical symptoms. RESULTS: Among the 198 patients with adrenal incidentaloma, nineteen patients were diagnosed with pheochromocytoma. Pheochromocytomas showed larger size and higher Hounsfield unit at precontrast computed tomography (CT) than did non-pheochromocytomas. All pheochromocytomas were larger than 2.0 cm, and the Hounsfield units were 19 or higher in precontrast CT. When both criteria of size > 2.0 cm and Hounsfield unit > 19 were met, the sensitivity and specificity for the diagnosis of pheochromocytoma were 100% and 79.3%, respectively. Compared with patients with pheochromocytoma, diagnosed based on typical symptoms, patients with incidentally detected pheochromocytoma were older, presented less often with hypertension, and showed lower levels of 24-hour urine metanephrine. CONCLUSION: Adrenal incidentaloma with < 2.0 cm in size or < or = 19 Hounsfield units in precontrast CT imaging was less likely to be a pheochromocytoma. Patients with incidentally discovered pheochromocytoma showed lower catecholamine metabolites, compared with those patients with symptomatic pheochromocytoma. -
Citations
Citations to this article as recorded by- Guidelines for the Management of Adrenal Incidentaloma: the Korean Endocrine Society, Committee of Clinical Practice Guidelines
Jung-Min Lee, Mee Kyoung Kim, Seung-Hyun Ko, Jung-Min Koh, Bo-Yeon Kim, Sang-Wan Kim, Soo-Kyung Kim, Hae-Jin Kim, Ohk-Hyun Ryu, Juri Park, Jung-Soo Lim, Seong Yeon Kim, Young Kee Shong, Soon Jib Yoo
The Korean Journal of Medicine.2017; 92(1): 4. CrossRef - Clinical Guidelines for the Management of Adrenal Incidentaloma
Jung-Min Lee, Mee Kyoung Kim, Seung-Hyun Ko, Jung-Min Koh, Bo-Yeon Kim, Sang Wan Kim, Soo-Kyung Kim, Hae Jin Kim, Ohk-Hyun Ryu, Juri Park, Jung Soo Lim, Seong Yeon Kim, Young Kee Shong, Soon Jib Yoo
Endocrinology and Metabolism.2017; 32(2): 200. CrossRef - Characterization of Incidentally Detected Adrenal Pheochromocytoma
Soon Jib Yoo, Woohyeon Kim
Endocrinology and Metabolism.2012; 27(2): 116. CrossRef
- Guidelines for the Management of Adrenal Incidentaloma: the Korean Endocrine Society, Committee of Clinical Practice Guidelines


 KES
KES

 First
First Prev
Prev



